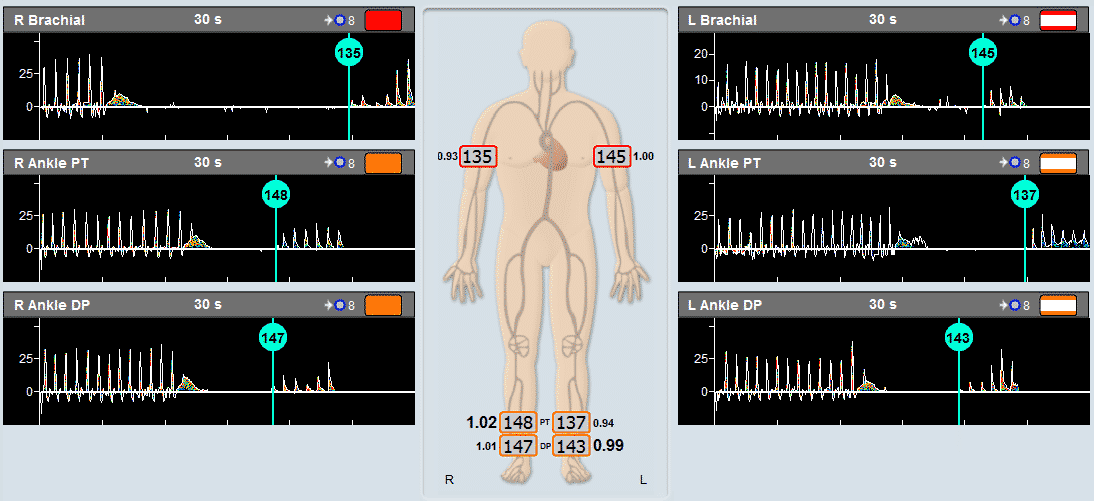
Q: When we perform ABI, our focus is to find the BP based on the waveform and the sound. Should we pay attention to or report the amplitude of the signal?
A: When perform ABI, it is important to focus on obtaining the best Doppler signal in order to accurately measure BPs.
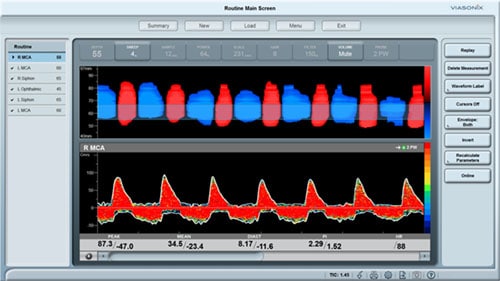
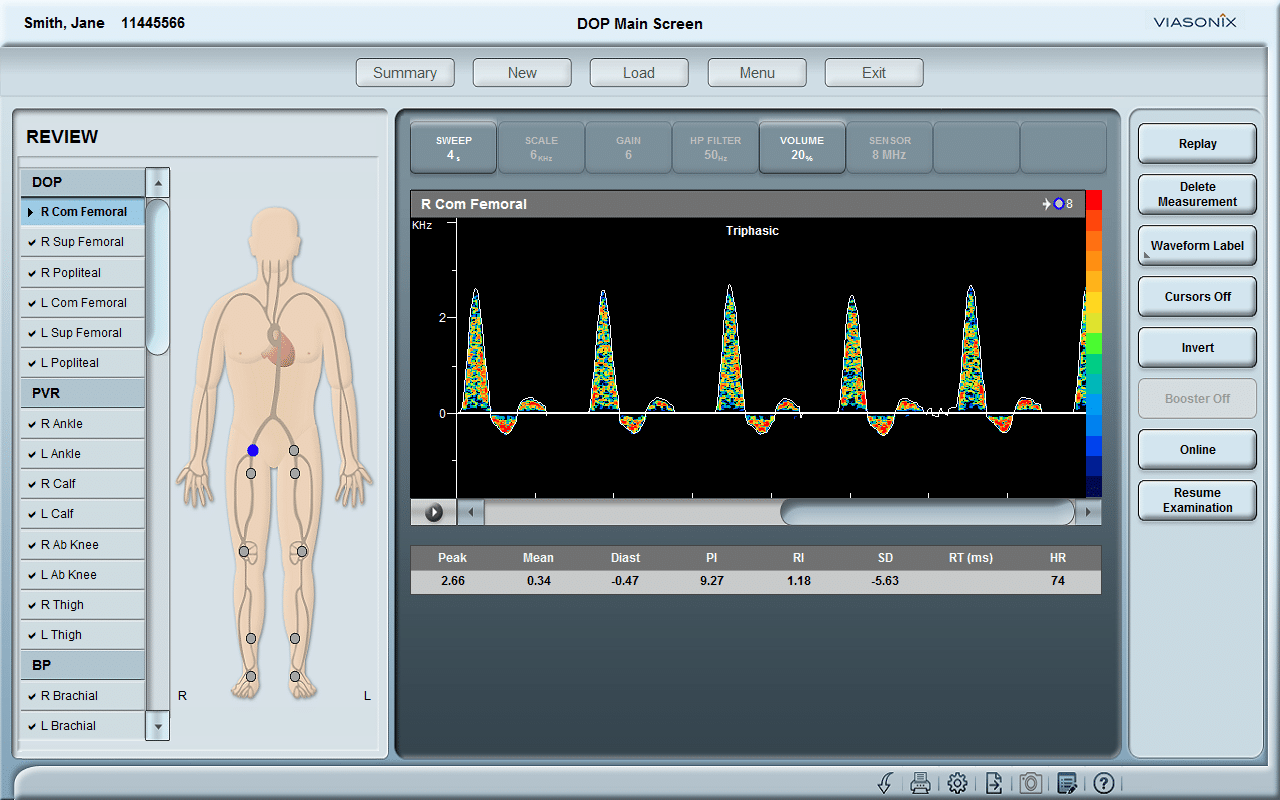
Spectral Doppler waveform assessment is a diagnostic tool used in the diagnosis of peripheral vascular disease. This consensus statement from the Society for Vascular Medicine and Society for Vascular Ultrasound gives useful information on interpretation of peripheral arterial and venous Doppler waveforms (https://doi.org/10.1177/1358863X20937665).
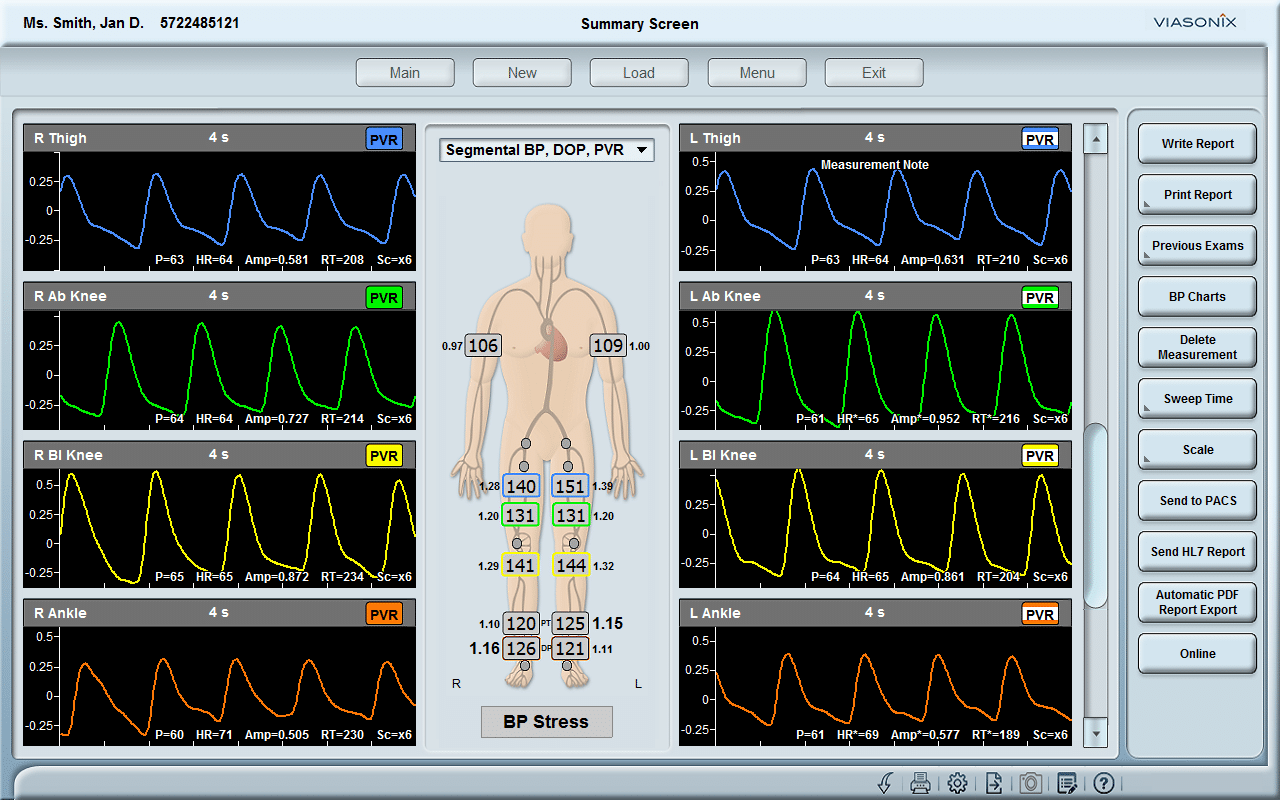
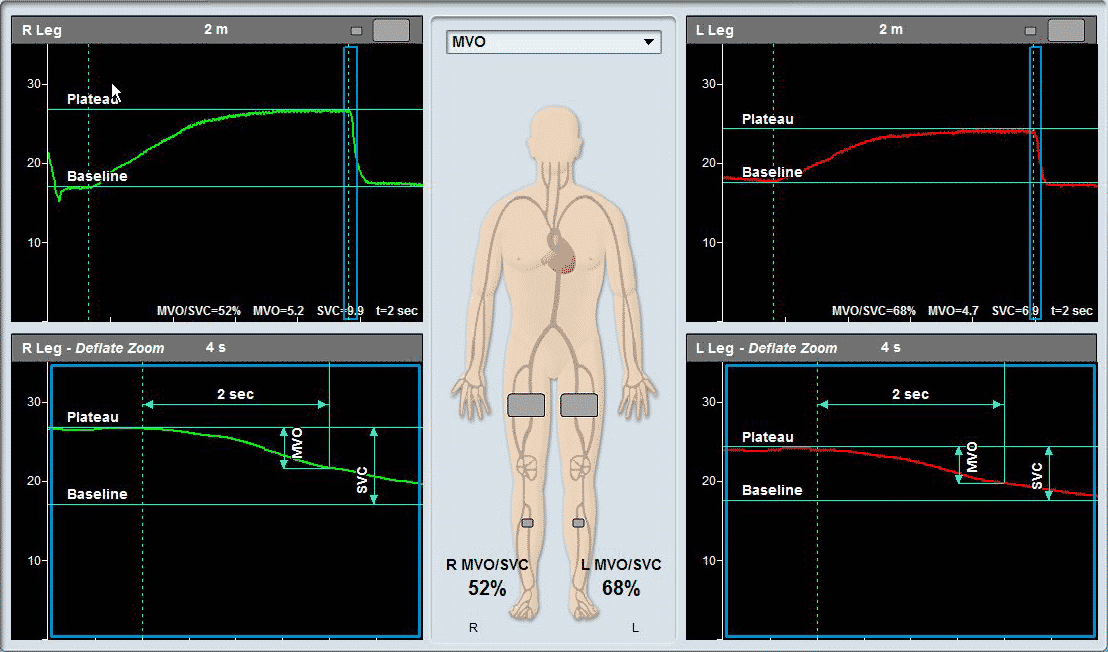
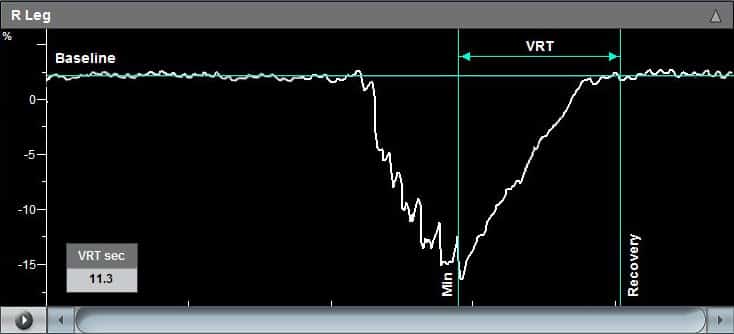
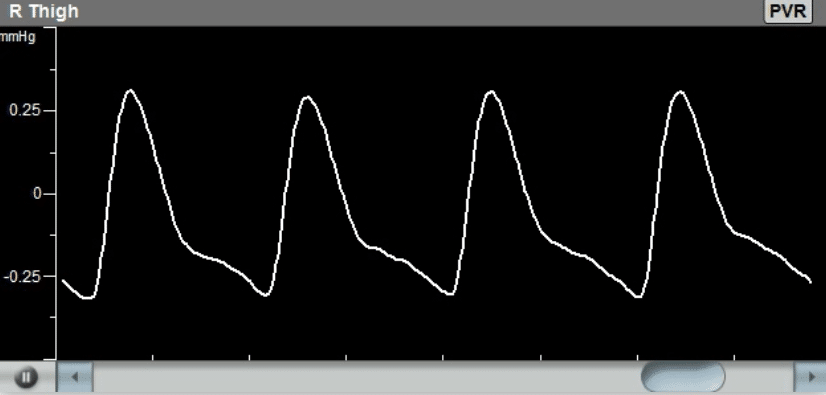
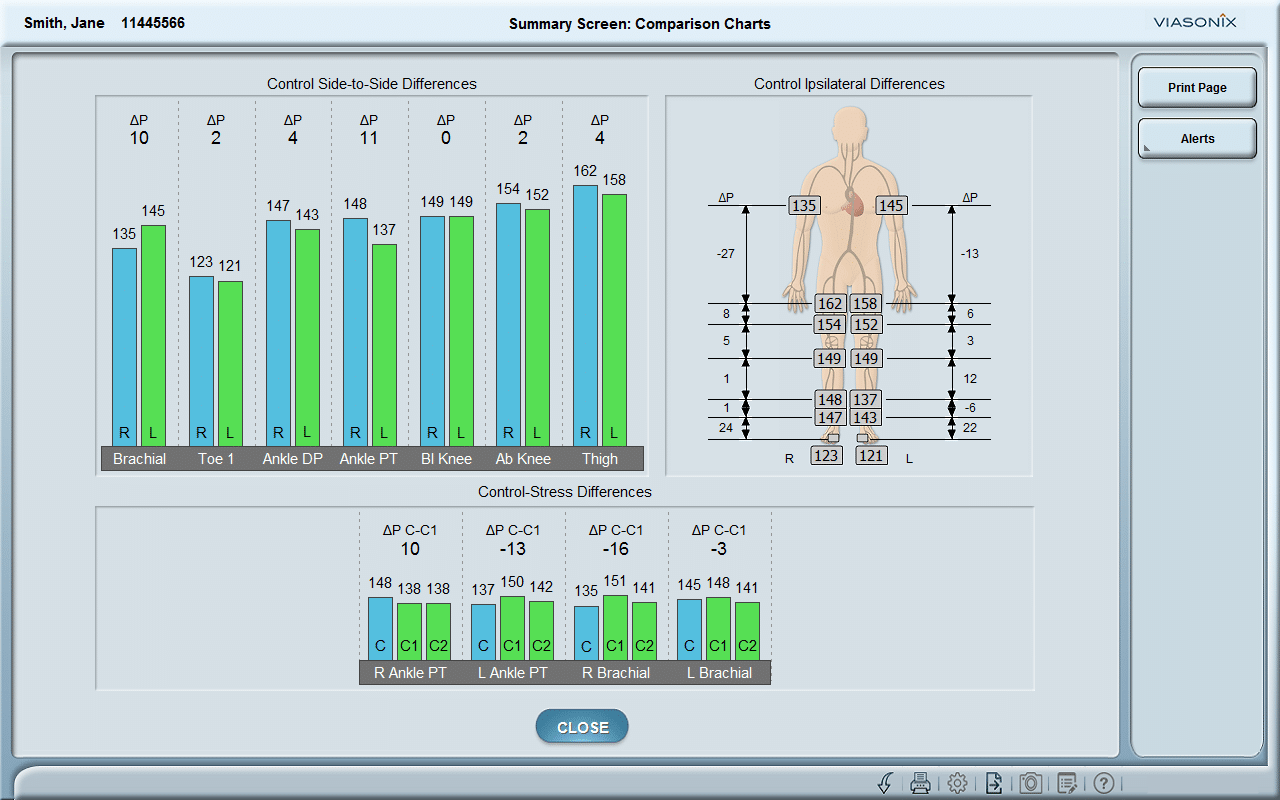
Q: When we perform PVR, should we report the waveform of the PVR or how to describe it in the report? Should we include the amplitude of the signal or the systolic rising time in the report? How reliable of these information?
A: Similar to Doppler waveform, PVR waveform assessment is useful in the diagnosis of peripheral vascular disease. This research report describes how to use PVR waveform analysis to identify inflow disease (https://doi.org/10.1177/8756479314548066).
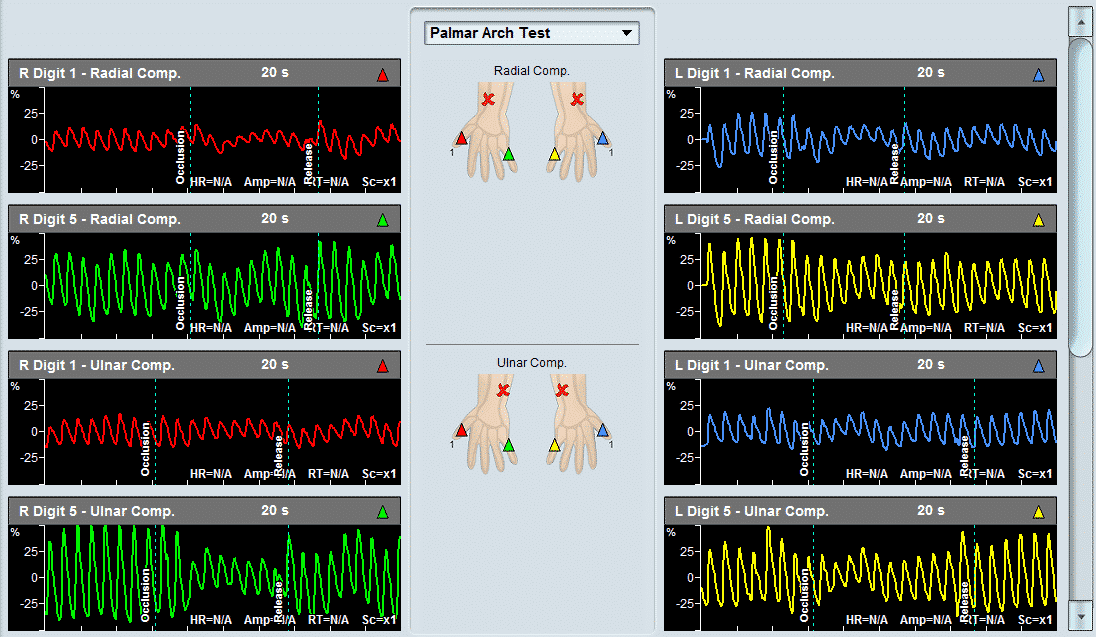
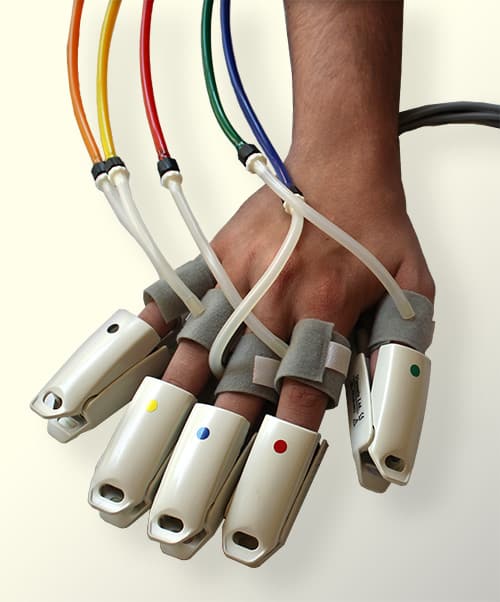
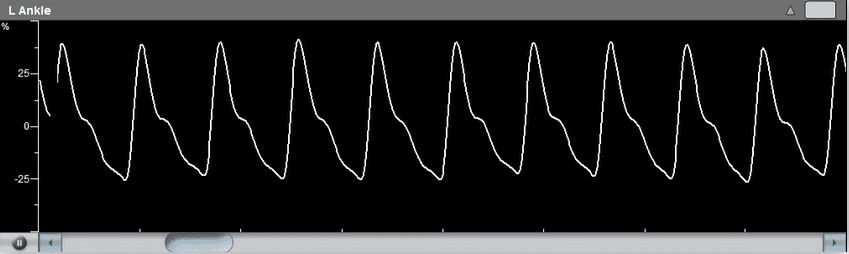
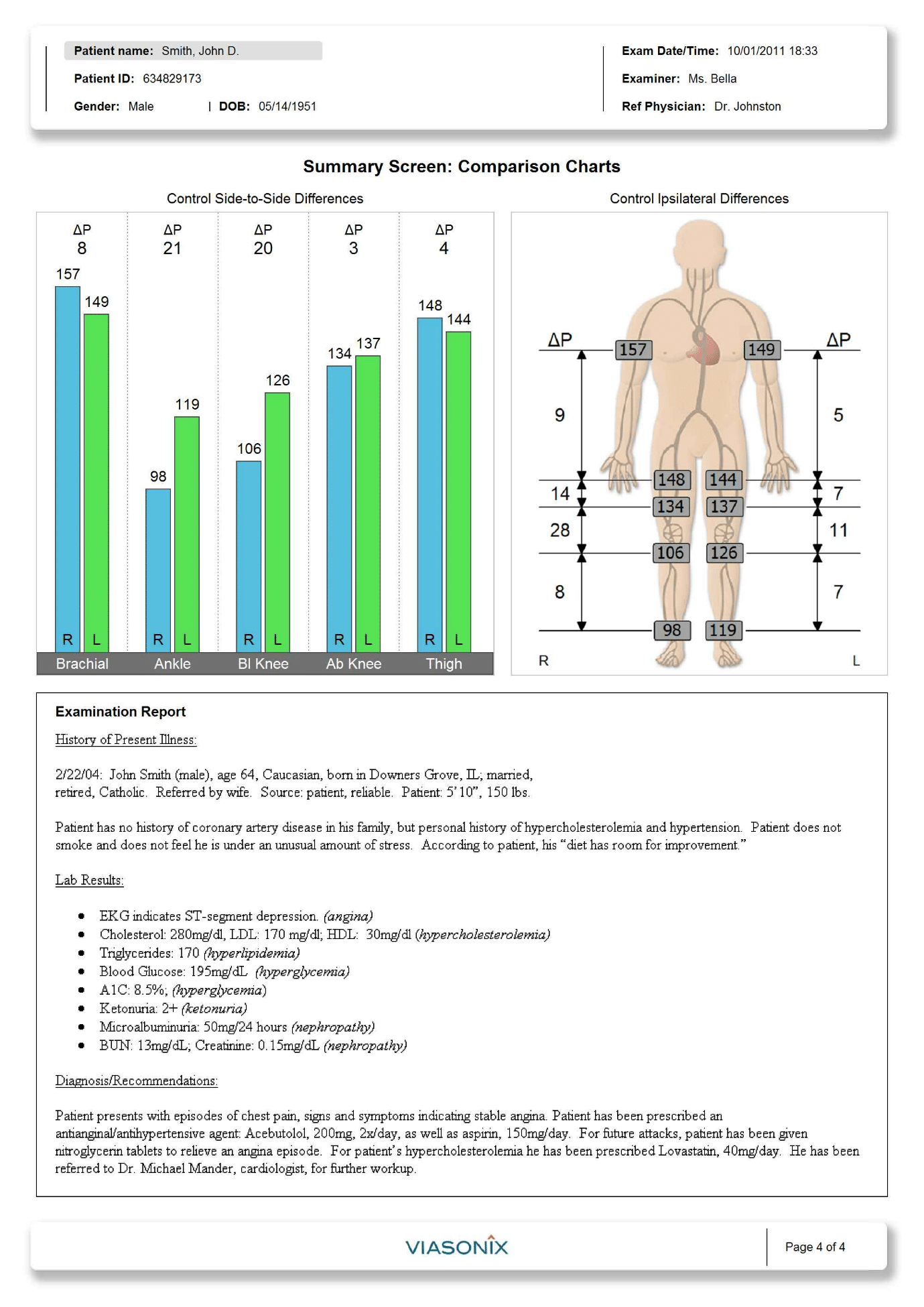
Q: When we perform TBI by using PPG in the dark, we normally focus the BP. Should we report the waveform or how to describe it in the report? Should we include the amplitude of the signal or the systolic rising time in the report? If the patient with 1st and 2nd toes amputated, should we proceed to other toes?
A: TBI is very useful especially when tibial arteries are incompressible. Additional toe waveform analysis may increase the accuracy of assessment for critical limb ischemia (https://doi.org/10.1016/S0741-5214(96)70101-5).
When patients have great toe amputated, you may proceed toe pressure measurement on other toes. However, you should remember results of most published studies on toe pressure are based on great toe. Furthermore, small toes may be too short to apply blood pressure cuff.
Q: The reproducibility of the toe waveform’s amplitude is quite poor and very often the amplitude is inconsistent with the ABI. Any suggestions to improve the reliability of the above tests.
A: 1) Every test has its limitations; 2) Practice makes perfect.
References:
- Interpretation of peripheral arterial and venous Doppler waveforms: A consensus statement from the Society for Vascular Medicine and Society for Vascular Ultrasound (https://doi.org/10.1177/1358863X20937665)
- Objective Lower Extremity Arterial Plethysmographic Waveform Characteristics for Differentiating Significant Inflow Disease in Nondiabetic Patients (https://doi.org/10.1177/8756479314548066)
- Value of toe pulse waves in addition to systolic pressures in the assessment of the severity of peripheral arterial disease and critical limb ischemia (https://doi.org/10.1016/S0741-5214(96)70101-5)